Can rheumatoid arthritis be prevented? (GS Paper 2, Health)
Why in news?
- Recently, a study proposed to repurpose an existing drug to treat rheumatoid arthritis as prophylaxis, to prevent disease.
- The results of the study showed that rheumatoid arthritis prevention trials are feasible and targeting the adaptive immunity of such individuals at an early stage, can prevent the onset of rheumatoid arthritis.
What is rheumatoid arthritis?
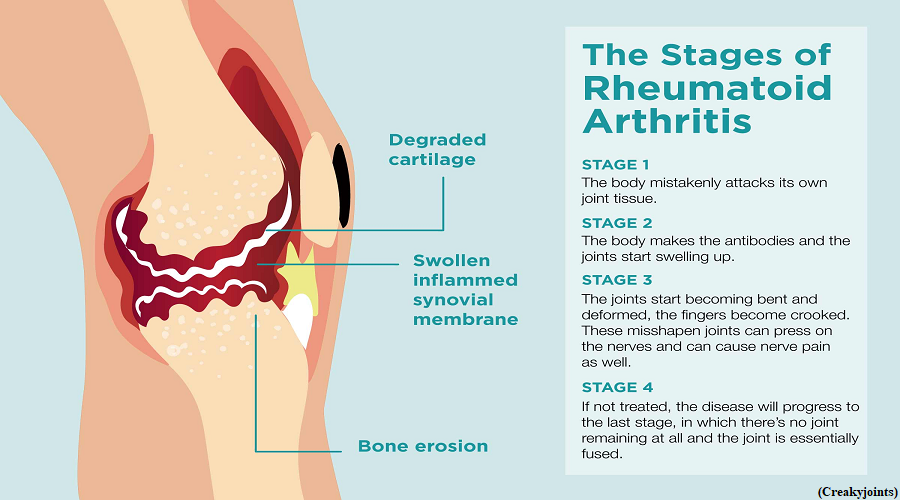
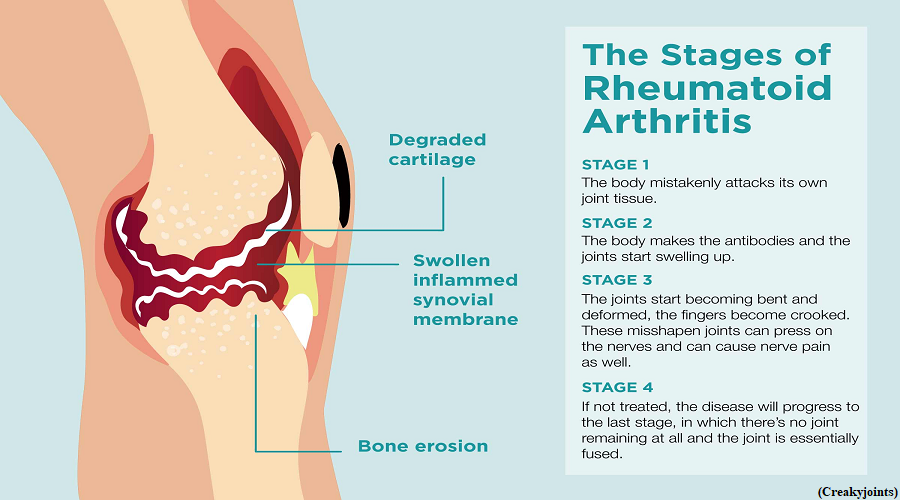
- It is a chronic, autoimmune condition that mostly affects the joints. Scientists have not yet understood why an autoimmune condition occurs, allowing the immune system that protects the body, to attack itself.
- A patient experiences pain, swelling of joints and loss of function and mobility as a result of stiffness. As can be expected, this is likely to significantly lower a patient’s quality of life.
- As per the National Institute of Arthritis and Musculoskeletal and Skin Diseases, of the National Institutes of Health, U.S., rheumatoid arthritis affects the lining of the joints, and damages the tissue that covers the ends of the bones in a joint.
- It often occurs in a symmetrical pattern, meaning that if one knee or hand has the condition, the other hand or knee is also often affected.
- Fatigue, occasional fevers, and a loss of appetite are to be expected, and there is a possibility that it may cause medical problems outside of the joints including in the heart, lungs, blood nerves, eyes and skin.
What did the study attempt to do?
- The idea was to evaluate the feasibility, efficacy, and acceptability of treating high risk individuals with an existing drug, Abatacept, to treat rheumatoid arthritis.
- The drug is a ‘co-stimulation modulator’ acting as a signalling pathway to start the appropriate immune response.
- At the core of their experiment is the understanding that individuals at high risk for rheumatoid arthritis can be identified years before they actually develop the disease, even as early as decades earlier, by detecting autoantibodies associated with rheumatoid arthritis known as Anticitrullinated Peptide antibodies (ACPAs), in the blood.
- Although the presence of autoantibodies might precede disease onset by a decade or more, the combination of ACPA with symptoms, and evidence of subclinical synovitis (inflammation of the lining of the joint) by imaging, has increased the predictive power of identifying individuals who are most likely to progress to rheumatoid arthritis within two years.
- These features have provided a framework for evaluating therapeutic strategies that could delay or prevent disease onset.
- The results show that rheumatoid arthritis prevention trials are feasible and targeting adaptive immunity at an early stage, with Abatacept, an existing drug for RA, before clinically apparent arthritis is manifest, can prevent the onset of rheumatoid arthritis.
- The drug of choice is Abatacept, a biological disease-modifying anti-rheumatic drug which works by selectively modulating signals to spur T-cell activation, or begin the body’s immune response.
What’s the Indian scenario with regard to rheumatoid arthritis treatment?
- Abatacept, a drug that comes under the classification ‘biologicals’ is no longer available in India; it was withdrawn after it did not sell well in the Indian market. But in the last five years, there have been six drugs to treat rheumatoid arthritis.
- At the moment, worldwide, 10 biologicals are available, and six of them in India. About three years ago, a group of drugs called JAK inhibitors came off patent, and one of those drugs, tofacitinib is available at ₹900 for a month’s supply.
- It is also an oral drug, as against biologicals that might be intravenous, or a subcutaneous injection, depending on which part of the world one is in.
Is early prevention of the disease significant?
- Pre-disease treatment with Abatacept reduces progression to clinically-apparent arthritis during the 12-month treatment phase, and up to 24 months after stopping treatment.
- However, by 24 months, the parameters of those who received the drug were similar to those with the placebo group; it was similar between groups, indicating that treatment is not sustained.
Smoking leaves a lasting adverse impact on immune responses
(GS Paper 2, Health)
Why in news?
- Smoking has a lasting effect on specific human immune responses, persisting long after quitting.
- The study, which investigates a range of factors that might contribute to variability in immune responses, also identifies body mass index (BMI) and latent infections of cytomegalovirus (a common virus) as having a substantial influence on immune responses.
- The findings offer insights into the factors that potentially underlie the risk of developing infections and other immune related illnesses such as cancer or auto-immune disease.

Response to immune challenges:
- There is wide variability in the way humans respond to immune challenges, such as bacterial or viral infections, as seen with the diverse range of clinical outcomes observed after infection with SARS-CoV-2.
- Age, sex and genetic factors play a major role in this variability, but modifiable environmental factors, such as lifestyle, may also contribute.
- Understanding how such variables affect immune responses could improve the design of treatments and vaccines.
Key Highlights:
- Researchers investigated the effects of 136 environmental factors on variability of immune responses in 1,000 individuals. Among the environmental factors studied, smoking was shown to have the greatest influence on immune responses.
- It affected both innate and adaptive immunity, the former is a general response whereas the latter is more specialized and pathogen-specific.
- While the effects on innate responses (such as increased inflammatory responses) were transient and lost after smoking cessation, the effects on the adaptive response persist for many years after quitting, altering the levels of cytokines released upon infection or other immune challenges.
- The results collectively show a short-term effect of smoking on innate immune responses, and a long-term effect of smoking on adaptive immune responses.
Findings:
- The study identifies a strong link between these previously proposed disease biomarkers and response to immune challenges in smokers versus non-smokers.
- BMI and cytomegalovirus are also found to have noteworthy effects on cytokine secretion, but the variance associated with smoking reaches levels equivalent to those linked to factors that cannot be changed.